-
PRODUCTS
- Anaesthesia & Respiratory
- Baby
- Casting
- Continence Care
-
Diagnostic
- See all Diagnostic
- Accessories
- Bladder Scanner
- Blood Testing
- Breathalyzer
- Cholesterol Testing
- Covid Testing
- Dermatoscope
- Diabetes Monitoring
- Drug Testing
- Endoscopy
- Eye Ear Nose & Throat
- Height Measures and Charts
- INR
- Jars and Containers
- Medical and Surgical Instruments
- Parts and Accessories
- Scales
- Testing
- Urinalysis
- Womens Health
- Ear Irrigation
-
Equipment
- See all Equipment
- "Miscelllaneous, Parts and Accessories"
- Beds
- Blood Collection Chair
- Bracket & Dispensers
- Carts & Trolleys
- Cryosurgery
- Electrosurgery
- Examination Couches & Tables
- Fridge & Freezers
- IV Stands
- Laundry & Cleaning Trolleys
- Miscellaneous
- Play Panels
- Privacy Screens and Curtains
- Stools and Step Ups
- Stools, Bed Screens & IV Stands
- Tens
- Transferring & Patient Handling
- Waste Disposal
- X-Ray Viewers
-
General Consumables
- See all General Consumables
- "Couch Rolls, Protectors & Underpads"
- "Registers, Records and Certificates"
- Bags Assorted
- Batteries
- Blankets and Warmers
- Bracket
- Child Rewards
- Containers
- Cups
- Dental Film Process Products
- Dr Bags
- Ear Piercing
- Feminine Hygiene
- First Aid and Trauma
- Gels and Lubricants
- Identification
- Linen
- Marker
- Miscellaneous
- Ostomy
- Paper and Printing Consumables
- Paper Products
- Parts and Accessories
- Personal Care
- Pill Cutters and Crushers
- Ultrasound Gel
- Wooden Applicators
- Gloves
- Hand & Body Hygiene
-
Infection Prevention & Control
- See all Infection Prevention & Control
- Absorbent Powder
- Bedpans & Urinals
- Caps
- Clinical Sheets
- Containers
- Dispensers
- Eye Protection
- Face Masks
- Hand Hygiene
- Miscellaneous
- Parts & Accessories
- Protective Apparel
- Scrubs
- Spill Kit
- Surface Cleansers & Wipes
- Surgical Packs & Drapes
- Toileting & Waste Disposal
- Tray Liners
- Wipes and Skin Protection
- Intravenous Infusion & Administration
-
Medical & Surgical Instruments
- See all Medical & Surgical Instruments
- Biopsy Punch
- Chiropody Pliers & Podiatry
- Cleaning and Protection
- Curettes
- Dental Syringe
- Dilator
- Ear Irrigation
- Forceps
- Hammer
- Male Health
- Marker
- Miscellaneous
- Nasal Speculum
- Needle Holder
- Pack
- Probe
- Retractor
- Ring Cutter
- Scalpel Handles & Blades
- Scissors
- Skin Hook
- Sucker
- Tuning Forks
- Urology
- Uterine Curettes & Sounds
- Medical Lighting
- Medical Lighting
- Needles & Syringes
- Nutritional Support
- Oral Care
- Patient Monitoring
-
Pharmaceuticals
- See all Pharmaceuticals
- Alimentary
- Anaesthetic
- Analgesia
- Antihistamines
- Cardiovascular
- Central Nervous System
- Creams and Ointments
- Endocrine & Metabolic
- Eye Ear Nose & Throat
- Infections & Infestations
- Miscellaneous
- Musculoskeletal
- Nutrition
- Ointment Products
- Other
- Register
- Respiratory
- Skin
- Solutions
- Rehabilitation & Mobility
- Skin Care
- Sports & Recovery
-
Sterilisation
- See all Sterilisation
- Autoclaves
- Biological Indicators and incubators
- Chemical Indicator Tapes
- Chemical Indicators and Integrators
- Cleansing Solutions & Detergents
- Instrument Protector
- Labels
- Marker
- Paper and Printing Consumables
- Parts & Accessories
- Record Keeping Supplies
- Steam Indicator Sheets and Tests
- Sterilisation Pouches & Rolls
- Towels and Cloths
- Trays and Bowls
- Ultrasonic Cleaners
- Water
- Wraps
- Sutures & Skin Closures
- Urology
- Vaccines
- Wound Care
- Wound Management
- News & Updates
24% of Chronic Kidney Disease (CKD) patients also have Peripheral Arterial Disease (PAD)
Understanding the Link Between Chronic Kidney Disease (CKD) and Peripheral Arterial Disease (PAD)
The Bidirectional Relationship Between CKD and PAD
- Hypertension
- Diabetes
- Smoking
- Overweight/Obesity
Early Detection and Diagnosis: Why Ankle-Brachial Index (ABI) Matters
ESC Guidelines 2017 recommended that patients at risk for atherosclerotic cardiovascular events should routinely have ABI measured. Similarly, KDOQI Guidelines support regular screening of ABI in patients with CKD, preferably those on dialysis. Regular surveillance of ABI not only aids in detecting arterial blockages but also prevents further development of PAD by improving management of both cardiovascular and kidney health.
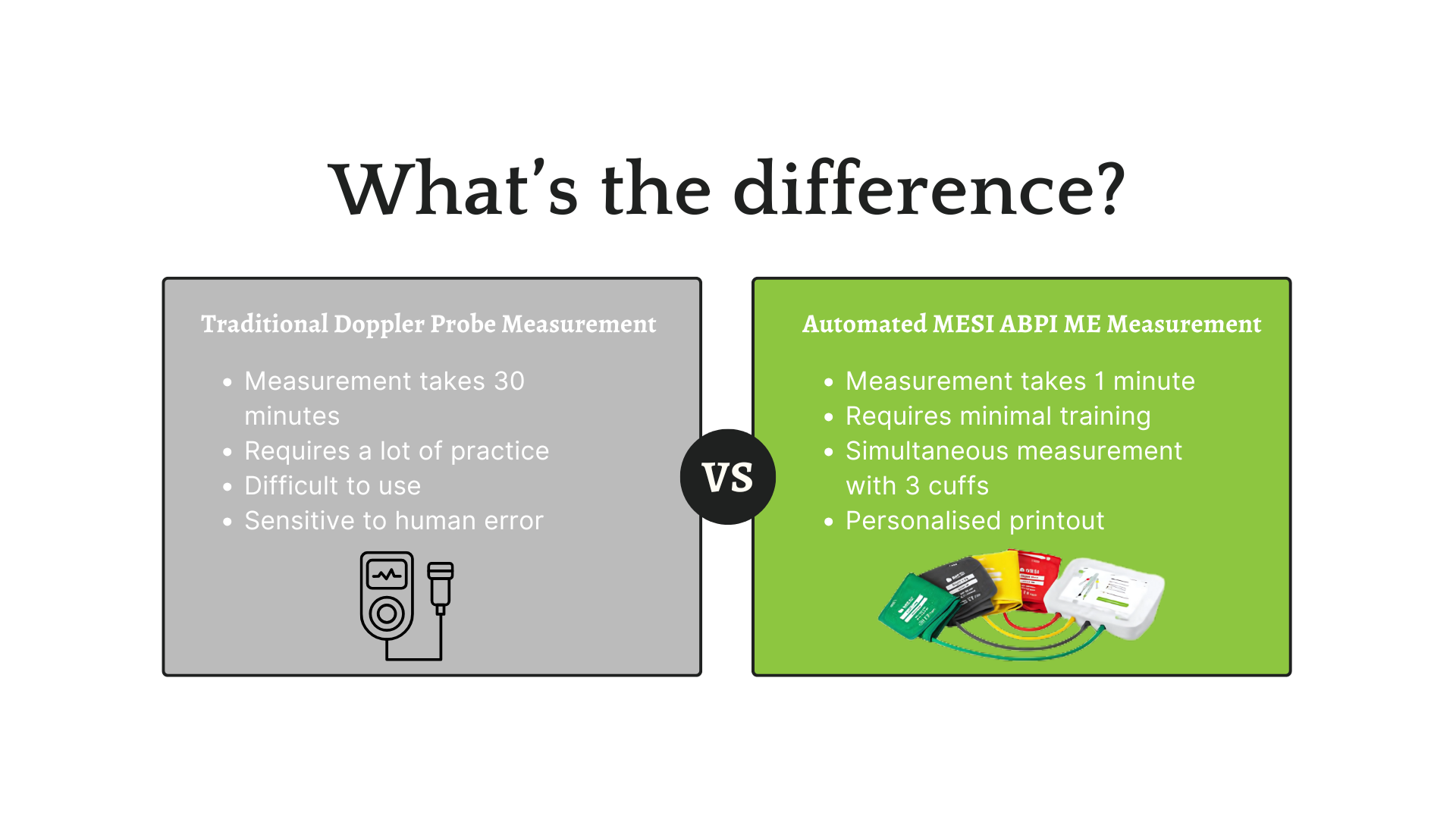
Simplifying ABI Measurement with Advanced Technology
Clinical Insights: The Importance of ABI in Vascular Health
The use of automated ABI devices finally allows the measurement of ABI in all dialysis patients without depriving other treatments of the critical time they need. This will finally permit a comprehensive vascular management, helping to lighten risks bound to CKD and PAD.
Learn More About MESI ABPI MD: A Revolutionary Tool for ABI Measurement
References
- Aboyans, V., et al. (2018). 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases. Revista Española de Cardiología (English Edition), 71(2), p.111.
- DeLoach, S., & Mohler, E. (2007). Peripheral Arterial Disease: A Guide for Nephrologists. Clinical Journal of the American Society of Nephrology, 2(4), pp.839-846.
- Garimella, P., & Hirsch, A. (2014). Peripheral Artery Disease and Chronic Kidney Disease: Clinical Synergy to Improve Outcomes. Advances in Chronic Kidney Disease, 21(6), pp.460-471.
- K/DOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients. (2005). American Journal of Kidney Diseases, 45, pp.16-153.
Newsletter
Please enter your email address to subscribe to our newsletters.